Introduction of each research theme
Dissecting the molecular mechanisms that maintain skin homeostasis
The surface of the skin is covered by the epidermis, where hair follicles and sweat ducts open, forming a barrier that protects our body from various external stimuli. Prof. Akiharu Kubo has investigated the mechanism of skin barrier homeostasis by mass spectrometric imaging of the stratum corneum barrier (Kubo et al, Sci Rep 2013), the interaction between the epidermal tight junction barrier and Langerhans cells (Kubo et al, JEM 2009), and the cell turnover mechanism with the maintenance of the tight junction barrier in the epidermis and sebaceous glands (Yokouchi et al, eLife 2016, Atsugi et al, JID 2020). At the Department of Dermatology, Kobe University, Prof. Kubo, Dr. Fukumoto, Dr. Akiko Kubo and our graduate students are investigating (1) the mechanism by which mutant cells replace normal epidermis from the point of view of cell competition, and (2) the structure of eccrine sweat glands and cell biological mechanisms of sweat-related diseases.
Interaction of Langerhans cells with the epidermal tight junction barrier.
In the steady state, Langerhans cells stay below the epidermal tight junction barrier.
When activated, Langerhans cells elongate their dendrites to penetrate the tight junction barrier and take up external antigens to establish preemptive immunity.
Epidermal cell turnover with maintaining the integrity of tight junction barrier
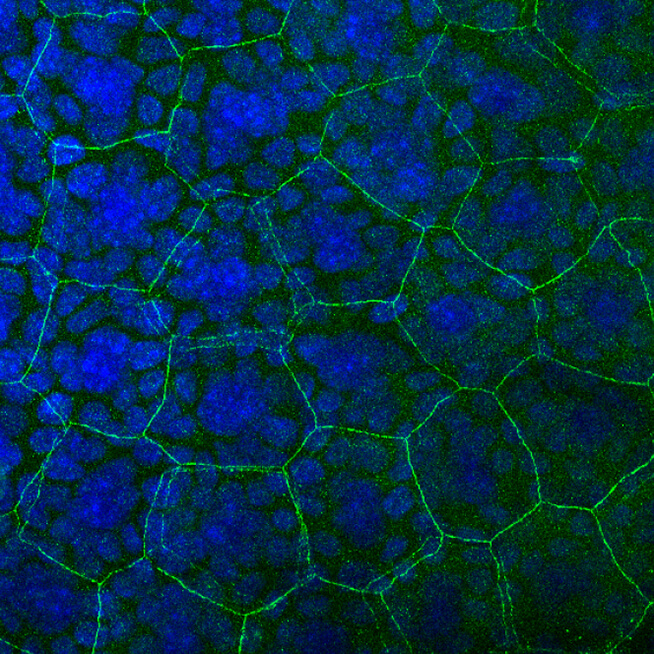
The replacement of epidermal cells occurs sequentially, with each cell’s replacement ensuring the maintenance of the epidermal tight junction barrier. This mechanism depends on the specific shape of the epidermal cell, the flattened Kelvin’s tetrakaidekahedron, a specific polyhedron characterized by 14 distinct faces.
The green lines observable between cells are known as tight junctions, which function to seal the space between cells. In the stratified epithelium, a single layer of cells is equipped with tight junctions, resulting in a honeycomb pattern comprised of a single green line. However, during the replacement of cells, a notable transformation occurs wherein the original green hexagon and the newly formed purple hexagon coalesce, resulting in a double hexagon. This mechanism ensures that new cells can be seamlessly integrated without compromising the integrity of the tight junction barrier.
Understanding and developing treatments for congenital and/or inherited skin disorders
There are 500 to 1,000 congenital and/or inherited disorders that manifest in the skin. We are conducting genetic analysis of congenital skin disorders using various genetic/epigenetic analyses including whole exome sequencing, SNP array and EPIC array for diagnosis and genetic counseling, as well as dissecting the pathogenesis and unidentified causative genes of the disorders. Prof. Kubo has achieved the discovery of the causative gene for Nagashima-type palmoplantar keratosis (Kubo et al, Am J Hum Genet 2013) and the elucidation of a novel causative gene, second hit-dependent pathogenesis, and epigenetic predisposition mechanism of porokeratosis (Kubo et al, JID 2019, Saito et al, Am J Hum Genet 2024). In the Department of Dermatology at Kobe University, Dr. Yoshioka, Dr. Akiko Kubo, together with graduate students, have worked on (1) development and analysis of mouse models of porokeratosis, (2) molecular dissection of cornoid lamellar formation, (3) identification of novel mosaic skin disorders, and (4) risk assessment of disease transmission to next generations in segmental (mosaic) cases of neurofibromatosis type I, in collaboration with Keio University, the National Center for Child Health and Development (NCCHD), and Yokohama City University.
The genetic and multi-omix diagnosis and
pathogenesis-oriented treatment of genodermaoses
There are 500 to 1,000 different congenital (hereditary) diseases in the field of dermatology, as well as mosaic diseases such as epidermal nevi, where symptoms only appear in one part of the body. In this study, we utilize a range of omics analyses, including whole exome analysis, whole genome analysis, and RNA-seq, to elucidate the genetic alterations that underpin the disease. We also provide medical care and genetic counseling, based on accurate diagnoses. Additionally, for diseases where the underlying cause remains unknown, we identify the genetic changes that contribute to the disease and gain insights into its pathogenesis.
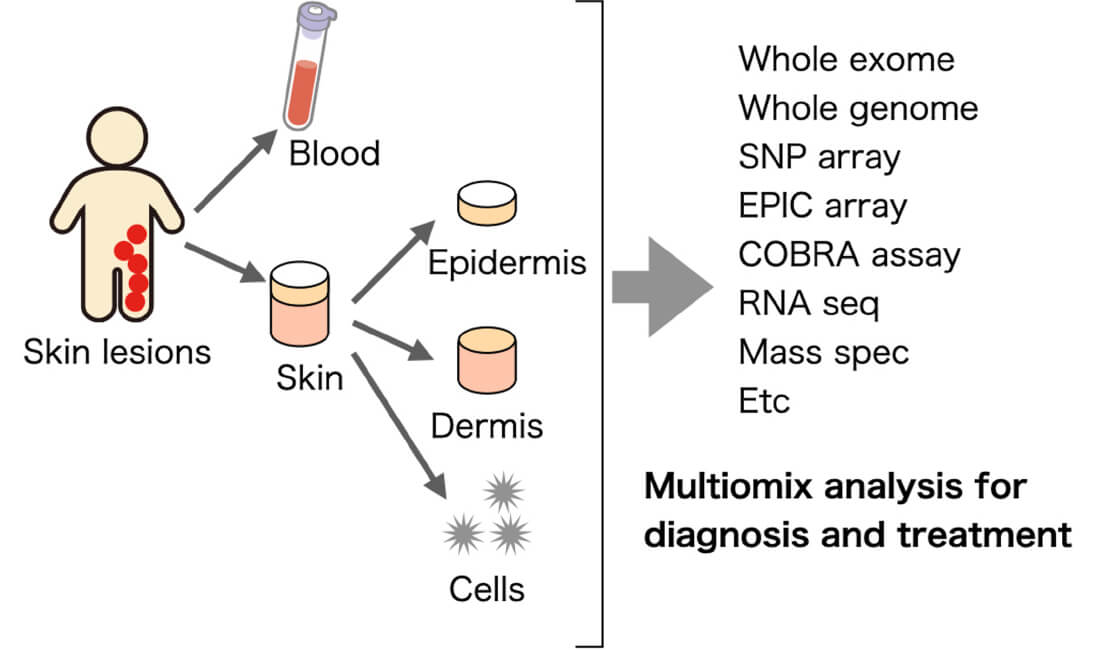
If you have patients with rare diseases or congenital (hereditary) skin diseases such as various types of nevi, hereditary tumors, congenital bullous disease, ichthyosis, and palmoplantar keratoderma, and have any questions about diagnosis or treatment, please contact us by email at the address below.
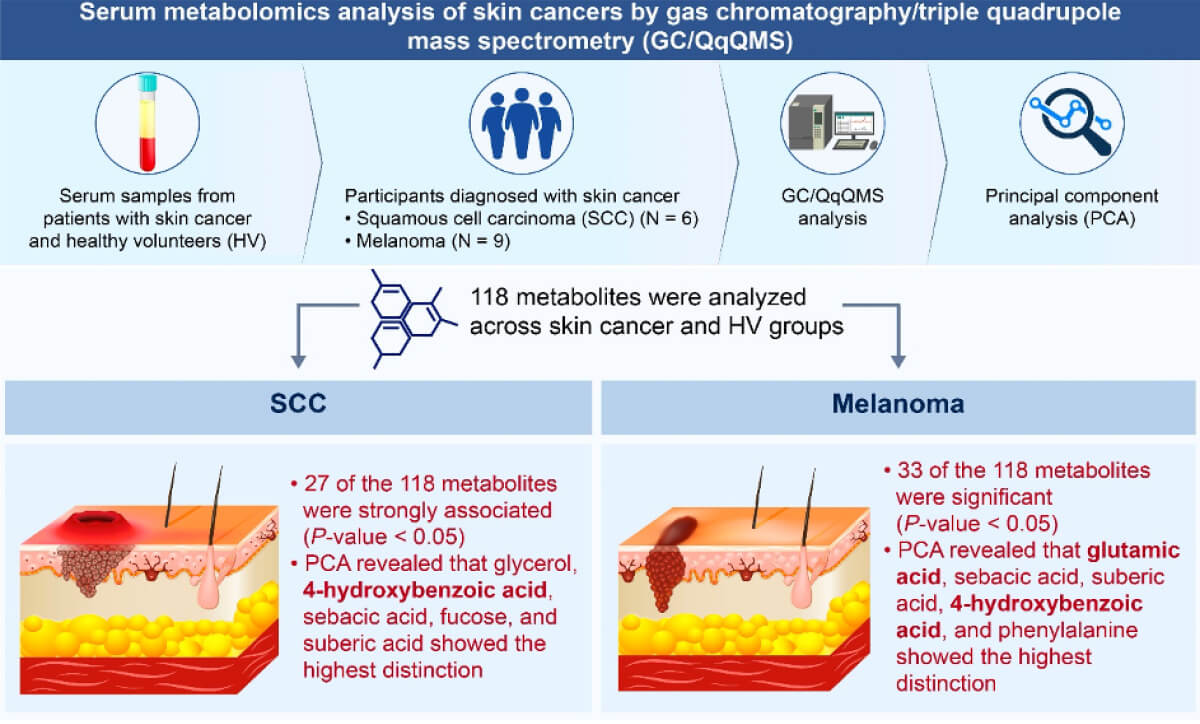
Exploring biomarkers using comprehensive genetic and
metabolomic analyses in skin cancer
Approximately 50% of the population will develop cancer at some point during their lifetime, with approximately 30% ultimately succumbing to cancer. The future of cancer treatment will be characterized by a shift towards personalized medicine, whereby the distinctive profile of each individual patient is elucidated and the most appropriate treatment approach is selected. The objective of this research is to identify biomarkers for the purpose of developing personalized treatments for skin cancer through the application of genetic and metabolomic analyses. Specifically, we are conducting whole-genome sequencing, exome sequencing, and targeted next-generation sequencing on tissue samples from malignant melanoma, extramammary Paget’s disease, and angiosarcoma. We are investigating the correlation between gene mutations and factors such as stage, prognosis, and tumor size. Additionally, we are analyzing the metabolome in the blood of the same skin cancer patients and comparing it with their treatment progress to identify biomarkers that can predict treatment efficacy.
An Intra-individual, Open-Label, Exploratory Clinical Study on the Efficacy
of Oxybutynin Hydrochloride Lotion for Dyshidrosis
Dyshidrosis is a condition where small, itchy blisters and redness appear on the palms and soles. Although topical treatments like corticosteroids have been used, many people do not experience relief, and there is no clearly effective treatment at present. In response, we have begun a study to examine the effects and safety of using oxybutynin hydrochloride lotion on patients with dyshidrosis. The goal is to see if it is effective and safe. If the results are promising, this could lead to larger studies and potentially help develop a future treatment for dyshidrosis.

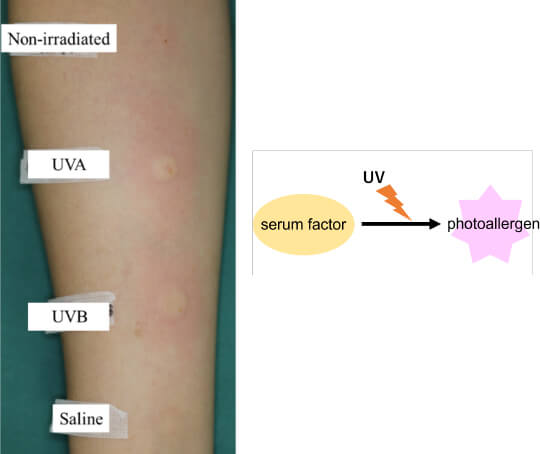
Identification photoallergens in solar urticaria.
Solar urticaria (SU) is a form of physical urticaria that presents with wheals following light exposure. The activating wavelengths responsible for SU vary among patients, including UVB, UVA, and/or visible light. Although it has long been postulated that factors in serum alter by irradiation to sunlight and act as autoantigens (serum photoallergens) in the pathogenesis of solar urticaria, the photoallergens have not been identified yet. Oda established the basophil activation test method to detect serum photoallergens in patients with SU in vitro (Oda Y et al, JACI in pra 2020). In the Department of Dermatology at Kobe University, we have established a registry of solar urticaria cases and studying the identification and analysis of endogenous photoallergens.
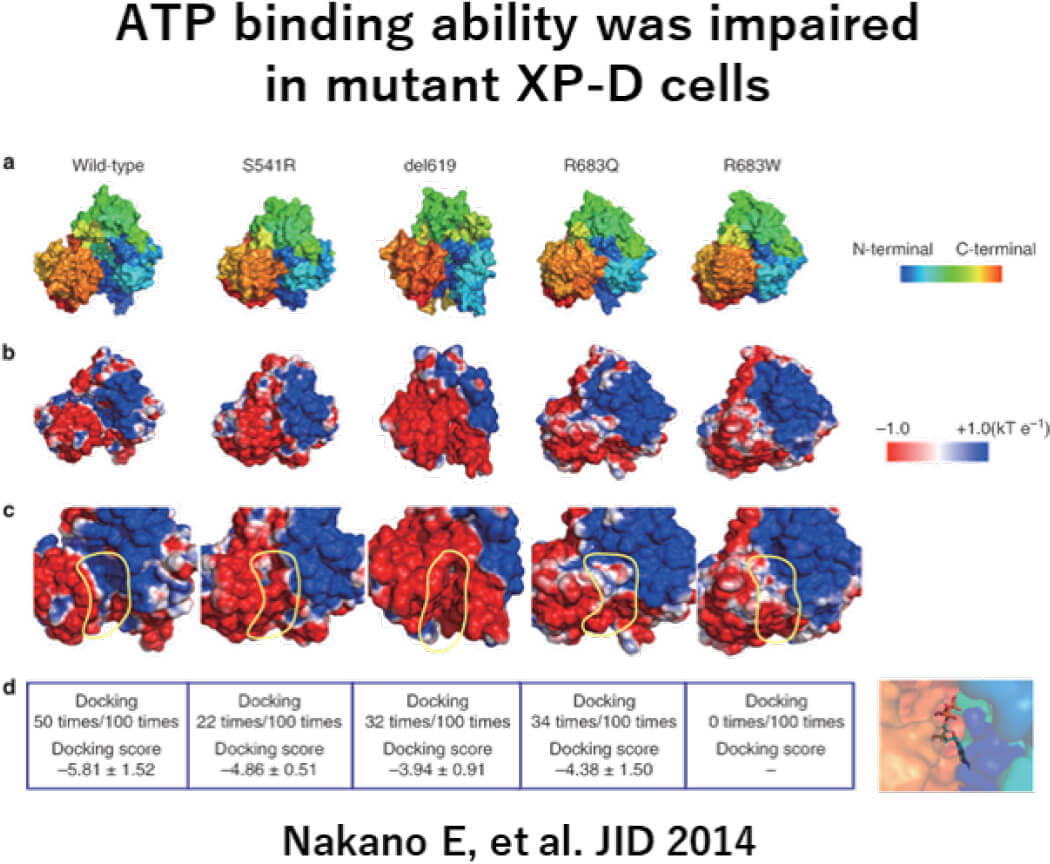
Elucidating etiologies and developing treatments for xeroderma pigmentosum
Xeroderma pigmentosum (XP) is an autosomal recessive disorder caused by dysfunction of factors involved in DNA damage repair. XP patients display severe hypersensitivity to ultraviolet radiation, and progressive neurological symptoms depending on the kind of disease and the site of genetic mutation. We have conducted research using XP cells and Xpa-deficient mice (Nakano E, et al. JID 2014, Kunisada M, et al. JID 2017, Nakano E, et al. JID 2018, Takeuchi S, et al. JDS 2022, Takeuchi S, et al. FASEB Bioadv. 2022). Based on these studies, we are conducting research aimed at elucidating the pathophysiology and developing treatments (Tsujimoto M, BMJ Open. 2023).
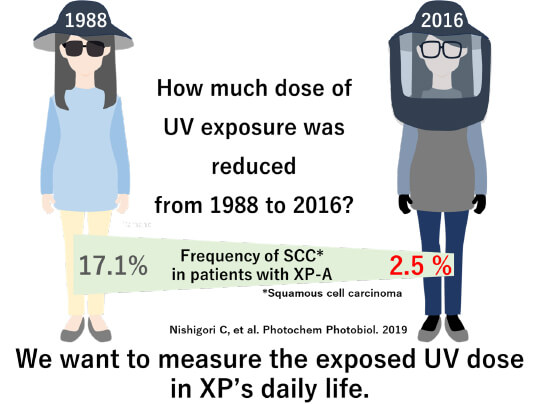
Development dosimeter for xeroderma pigmentosum patient
DNA damage occurs to a specific base sequence when the skin is exposed to ultraviolet radiation. Xeroderma pigmentosum (XP) patients do not have a suitable mechanism for repairing DNA damage.
As DNA damage accumulates, the risk of skin cancer increases.
It has been reported that XP patients have the risk of skin cancer 2,000 to 10,000 times higher than healthy people. For this reason, XP patients need to avoid ultraviolet radiation altogether every day.
In graduate school, Yamano studied the effects and safety of UV lays at each wavelength with the researcher of an optical company. (Yamano N et al. Photo Photo 2020, Yamano N, et al. Photo Photo 2021)
Using that experience, Yamano connects XP treatment and optical technology and develops a dosimeter to help protect xeroderma pigmentosum from ultraviolet radiation. This research is being conducted with the Department of Medical Device Engineering and optical technology companies.